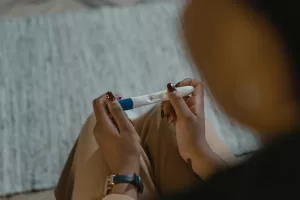
There’s little evidence to suggest that children conceived as a result of fertility treatment are at any greater risk of pregnancy complications or worse birth outcomes than their naturally conceived peers, finds a long-term study, published in the open access journal BMJ Medicine.
Although this method of conception is associated with fewer pregnancies, social rather than clinical factors may very well explain this, suggest the researchers.
The use of fertility treatment is increasing. And more than 10 million babies have been born worldwide using assisted reproduction techniques.
It’s known that the resulting pregnancies are at higher risk of several pregnancy and birth complications, although it’s not clear if these risks are associated with the treatment involved or the lower fertility.
Similarly, whether these risks might also affect the children conceived this way when they want to become parents themselves, isn’t clear either.
To explore this further, the researchers drew on the reproductive histories of more than 1 million Norwegian residents born between 1984 and 2002 and a pregnancy registered with the Medical Birth Registry of Norway up to the end of 2021.
They focused on various key indicators of newborn and maternal health. These included: average birth weight; gestational age; placental weight; risk of congenital birth defects; vital signs at birth (Apgar score); need for neonatal intensive care; caesarean section delivery; use of fertility treatment; high blood pressure and pre-eclampsia during pregnancy; premature birth; and the baby’s sex.
Among 1,092,151 people born in Norway from 1984 to 2002, some 180,652 were registered at least once as mothers and 137,530 as fathers.
Of these, 399 men out of a total 5083 (8%) conceived after fertility treatment and 553 women out of a total of 4763 (12%) had at least one registered pregnancy.
Analysis of the data showed little evidence that people conceived as a result of fertility treatment were themselves at heightened risk of the studied pregnancy or birth complications, or of assisted reproduction.
But conception after fertility treatment was associated with an 86% heightened risk of a low neonatal Apgar score among women conceived in this way, although the actual numbers were small. And the odds of having a boy were also 21% lower in this group.
People conceived after fertility treatment were also slightly (9-12%) less likely to have a registered pregnancy within the monitoring period (2002-21).
The researchers acknowledge certain limitations to the study findings, including the small number of pregnancies among people conceived after fertility treatment and the lack of information on potentially influential sociodemographic factors.
And given that all parents were born in Norway, the findings may not be more widely applicable to a more ethnically diverse population, they point out.
But they nevertheless state: “People conceived by assisted reproductive technologies were not at increased risk of obstetric or perinatal complications when becoming parents.”
And they explain: “Men and women who were conceived by assisted reproductive technologies had fewer pregnancies compared with their peers who were naturally conceived, which might be attributable to social factors.”
Larger studies with a longer monitoring period and more direct assessment of time to pregnancy are needed to confirm their findings and evaluate the pregnancy outcomes for older parents who were conceived after fertility treatment, they suggest.
“Meanwhile, these early results are reassuring for the increasing number of adolescents and young adults who were conceived by [assisted reproduction] and are entering their reproductive years,” they conclude.
Source:
Journal reference:
Carlsen, E. Ø., et al. (2023). Reproductive outcomes in women and men conceived by assisted reproductive technologies in Norway: prospective registry based study. BMJ Medicine. doi.org/10.1136/bmjmed-2022-000318.