Welcome to The Betty Rocker Show! I’m so glad you’re going to listen to this episode today. My doctor and friend Dr. Jill Carnahan is back to talk to us about the most important lab tests you should get for your health from a functional medicine doctor’s perspective.
Welcome to The Betty Rocker Show! I’m so glad you’re going to listen to this episode today. My doctor and friend Dr. Jill Carnahan is back to talk to us about the most important lab tests you should get for your health from a functional medicine doctor’s perspective.
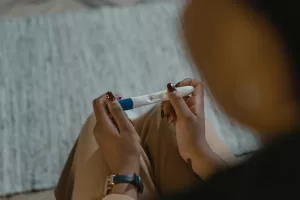
PLUS, we’re talking about the best way to test your hormones to see where your levels are at, and the different types of hormone balancing treatment options – pros and cons, and how to stay on top of it so you can feel your best (this starts about halfway through the episode if you’re looking for it!).
You can ask your doctor to get these tests for you, and we also share some direct-to-consumer labs that offer affordable testing, like Vital Health and Rupa Health.
We’re also digging into the aftereffects of COVID on women in peri and post menopause, as this is something that is just starting to be addressed and understood and personally affected me and many of Dr. Jill’s other patients as well.
Remember, you can reference back to the transcript anytime if you can’t remember something she said, or you were taking notes and you weren’t familiar with a term. You can find it right in the transcript notes.
Dr. Jill has a NEW BOOK out called Unexpected: Finding Resilience Through Functional Medicine, Science and Faith that introduces a new paradigm for readers who are going through uncertain times. Dr. Jill’s compassionate exploration of healing through functional medicine demonstrates how to replace darkness and fear with hope and find profound healing, unconditional love, and unexpected miracles in the process.
Unexpected reveals practical advice that can be used for conditions like mold and biotoxin illness, cancer, autoimmune disease, Lyme disease, and more. Dr. Jill’s raw and honest account of her own challenges facing breast cancer, living with autoimmunity, and mold toxicity, while working in a medical system that has little tolerance for stepping outside the lines, offers a new path of empowerment for taking control of your health and wellbeing.
Episode Transcript
(00:02):
Welcome to the Betty Rocker Show, the place to be, to nourish your mind, love your body, and rock your life.
Betty Rocker (00:20):
What’s up rockstars? It’s great to be with you. Today we’re welcoming Dr. Jill Carnahan back to the show to talk about some things that have been on my mind to share with you, including what blood tests do we really need to get a good snapshot of our health? Can we get them from our doctor? And how affordable are they really? I’m also talking to her about the different hormone treatments available for women who have imbalanced hormones, the pros and cons of the different types of treatments available, and how frequently you should test your hormones once you start a treatment plan. Plus, I’ve been super interested in how Covid affects our hormones and our immune system, and how this is playing out for women at different life stages. Now, if you haven’t heard of Dr. Jill Carnahan before, she’s the functional medicine doctor I trust and work with personally for my own healthcare.
(01:13)
Her clinic specializes in searching for those underlying triggers that contribute to illness, through cutting-edge lab testing and tailoring the intervention to specific individual needs.
She just released her new book, Unexpected: Finding Resilience through Functional Medicine, Science, and Faith, where you can read more about her incredible journey through facing breast cancer at 25, autoimmunity and mold toxicity while working in the conventional medical system. And her book shares her protocols for environmental toxicity and mold related illness, autoimmune disease, Lyme disease, and countless other complex chronic symptoms from over 20 years experience practicing functional medicine.
You can read this book and you can also learn a ton from listening to today’s conversation about the topics I mentioned we’re going to talk about. So join me in welcoming this amazing woman back to the show.
It’s so great to have you here.
Dr. Jill Carnahan (02:14):
Thank you. Always good to be with you and your awesome energy.
Betty Rocker (02:19):
It’s just such a treat to have you back. People were talking about our last couple of conversations. The first conversation we had, we talked about mold, and both of us have had that personal experience with it. I was fortunate enough to have you as my doctor going through healing from mold. And our last episode we talked about a lot of women’s health topics and there’s just so much we could cover because you’re an amazing functional medicine practitioner with such a wide breadth of knowledge. I don’t even know how you have time to fit this in with all your patients. How long is your waiting list right now? Last I heard it was three years long or something. You’re so popular.
Dr. Jill Carnahan (03:06):
About five years. Yeah.
Betty Rocker (03:08):
Right. Yes. I feel very, very lucky. But that’s again why you’re writing books, you’re putting out publications on your blog. You’re talking on podcasts. You’re out there sharing the information that you use in your patient practice, which is so valuable. So thank you again for coming back.
Dr. Jill Carnahan (03:27):
You’re welcome. Thank you. It’s actually like I would do it if I didn’t get paid, right? It’s one of those things that I know I’m called to do in this world. So thank you.
Betty Rocker (03:36):
That’s so true. And speaking of your amazing blog, which everyone should check out over on drjillcarnahan.com. You had a recent article that I shared in my group. I was talking about with a lot of friends. You were talking about the tests that everyone should get, the types of testing that people should get. And I think this is a topic that… A lot of us are really lost, unless we have a practitioner like yourself or someone who’s really educating us on what types of tests are important. And then maybe how do we ask for these tests, and then how do we read these tests and what’s important to know? I guess that’s my question to start us out is, what tests should women specifically be getting at, maybe different ages, and what are your recommendations in that regard?
Dr. Jill Carnahan (04:23):
Okay, I love this, and I did write recently about this. So it’s all out there for free if you want to just resource or whatever. But the bottom line is so often [inaudible 00:04:31], it seems like this unattainable thing where you might have heard, “Oh, this sounds great, but my insurance doesn’t cover it, and I can’t find any doctor that’s available at my space.” So what I want to do is give you… And most of these that I’m going to talk about are actually ones you can do through your insurance. So a lot of the comments I had when I wrote the blog and posted it were like, “Oh my gosh, that’s totally unavailable for the average person.” That’s not true. And that’s why I wrote it, because these are things that LabCorp Quest, your hospital lab, I’ll tell you which ones are and which ones aren’t, but most of them are completely available.
(05:02)
Now, the other thing is getting a doctor to order them. That could be an issue because say you’re in a HMO, the doctors are capped at what they can do and they’re often like, “You need to have this symptom in order to order this lab.” So they might be wanting to help you, but they are handcuffed a little bit by the system. But nowadays, there are direct to consumer labs and there are many, many platforms. I don’t even want to start naming because I don’t want to play favorites. But if you look up direct to consumer labs, you can often order these yourself for a fraction of the cost. And what people don’t know is say you take LabCorp Quest or any major lab, the lab rate they charge the insurance is literally almost 10 times what the actual price is.
(05:43)
So for example, if I order a huge panel of all these labs, it could be $8,000 that’s billed to the insurance. And everybody’s like, “Oh my gosh, that costs so much.” Well, first of all, if you have a normal good insurance plan that covers regular labs, that 8,000 will be deducted to 800, and then taken into your insurance, it goes toward your deductible or whatever, and you might be billed $200 or nothing. So it’s very, very tricky because these companies are making money and they’re building at a high rate because they know they’re going to get denied. If you directly go to my local hospital, which gives direct to consumer prices, that $8,000 bill will be about a 10th, somewhere between 500 or $800, which is still a lot. But I’m talking about a load of labs like loads and loads. So you can just-
Betty Rocker (06:26):
Right. You’re giving one example for specifics. And as someone who’s gone through this, I have to say what you’re saying is exactly right because I’ve had… So specifically, I’ll say which labs or the direct consumer, you tell me if I’m saying the right ones. Vibrant America was one of the ones that I used. And another one, it starts with an R, it’s Ru… What is it? Ru…
Dr. Jill Carnahan (06:49):
Rupa.
Betty Rocker (06:49):
Rupa Health. Yep. So there’s two right off the bat that I’ll say, you’re not playing favorites. I’ll just say two that I’ve had the experience with that are direct to consumer and those… So what you’re saying is really true. You can actually get your insurance to cover it, because I think… I’m so glad you addressed that elephant in the room. It’s like people hear about these great things and then they’re like, “Oh, but that’s not attainable for me.”
Dr. Jill Carnahan (07:13):
Not accessible. And I’m saying it isn’t. When I talk about large number, which is $8,000, it’s built the insurance maybe in, that’s talking a massive workup at an incredible depth. If you still just want this basic stuff, we’ll start with CMP, CBC. I’ll explain what these are in just a moment. And basics, you can go to local hospital and get it for a 150, somewhere between 75, $150. So you can get these for very reasonable costs and that’s outside of an insurance. If you go through your insurance, it’s often discounted. And thanks for letting me frame that because I want you to know as a listener, this isn’t necessarily unaccessible or only for the wealthy. It is absolutely accessible and you can decide how deep you go and how much you pay. So thanks for letting me share that.
Betty Rocker (07:57):
No, a hundred percent. And also… So maybe what’s the next framework that we should offer? Which age group do we want to talk… Maybe you would say different age groups would need these specific labs or these specific lists of things. So get out your pen and paper guys or take notes in your phone if you’re interested in some-
Dr. Jill Carnahan (08:16):
And I’ll go into detail here in a minute. I love that. When I wrote the 15 lab tests you should have by the age of 30, I just picked this average age of where… In our twenties, we think we’re invincible. I happened to get cancer at 25. But up until the cancer, I was like, “I’m great. I’m never going to…” We think we’re immortal, basically. There’s no… We’re thriving everything. 30 starting to be the point, somewhere between 30 and 40 where we start to be like, “Oh, I’m waking up a little sore in the morning,” especially after 40. So I would say absolutely, if you haven’t gotten an in-depth workup and you’re 40 or above, this is for you. But I think it’s more important to see patterns of where you’re walking towards on your trajectory towards health or disease, because often you can start to see abnormal patterns in your thirties, even though you feel great. And so this is preventative. You’re looking at these patterns before you ever get… because by 40 or 50, there’s some inset things that you might have more trouble reversing.
Betty Rocker (09:09):
Makes sense. So that was a great article. So if you’re in your thirties and you have the opportunity to get this lab test that Dr. Jill’s going to go over right now, great. If you haven’t had anything like this and you’re in your forties or fifties, this would probably still be very appropriate for you. If you… just to get some baseline numbers and then you could tell us what to do in the future to follow-ups. Okay. So that’s a great framework. Thank you.
Dr. Jill Carnahan (09:34):
And if you’re a motivated 25-year-old, by all means it’s perfect for you too, but you’re probably going to come up pretty normal because you haven’t yet had that time and exposure and everything. One thing on that real quick too, I keep going on these tangents, but I think they’re important. You could be born with a genetic predisposition towards something like celiac, but the average age of diagnosis is 55 years old. Because what happens is over the years, you might start to have inflammation, start to have inflammation, thirties, forties, and it takes an accumulation or a load of environmental toxicity of gluten in the case of celiac and thinks to actually manifest as full-blown disease. So the reason we’re saying 30 and above start this testing is because we want to predict where you’re headed and turn your course around, change course so that you don’t ever go to diabetes or you don’t ever go to gout or these things that we can actually prevent.
Betty Rocker (10:26):
Amazing. Great advice.
Dr. Jill Carnahan (10:30):
Okay, so let’s dive in. So CMP is a Comprehensive Metabolic Panel.And this is a basic thing that looks at your liver function, your kidney function, your absorption of nutrients and proteins, your electrolytes, and even calcium. So it’s a really basic metabolic panel, and it’s something that most doctors probably have ordered. So it’s not something that you would be shocked, like your doctor would be probably willing to order this. At a lab that’s doing a cash pay price for this, it’s probably about $10. So it’s that cheap to do. Complete blood counts, this is where you look at platelets. Platelets can cause clotting issues and if they’re too low, you’re going to have bleeding risk. If you’re too high, there’s inflammation or risk of clot. It looks at hemoglobin. So if you’re anemic or B12 deficient or have chronic inflammation that’s causing some reason to have low hemoglobin, it might be a reason to explain fatigue that’s all part of the CMP.
(11:33)
And then white blood count, I look at specifically because if you have a chronic infection like Lyme disease or Epstein-Barr, you can have a chronically low white blood count and many doctors be like, “Oh, that’s just normal for you.” And if I see a… say it’s a 3.0, which is low, usually the normal, somewhere between 4.5 and above, I’m looking for a chronic infection in that patient or something that’s creating a stress on the immune system. So again, a lot of docs will order this, this one will probably be about $15 cash, so pretty affordable. Advanced lipid profile, there’s many different forms of this, but the main thing here is you get the cholesterol, the LDL, the HDL, the triglycerides, the oxidized LDL, the apolipoprotein B, and the lipo A. This itself is a whole two-hour lecture, but the bottom line is this, cholesterol is not all bad.
(12:20)
Cholesterol is a precursor for all of our brain. Our brain is actually made of fats and cholesterol. It’s a precursor of all of our hormones including adrenal, thyroid and endocrine hormones. And so if we have too low of cholesterol, we can actually be deficient in hormones and things that we need to survive. So it’s important to find this balance. The problem with cholesterol isn’t just pure cholesterol, the problem is oxidized cholesterol. So if you have reactive oxygen from stress from our chemicals or things that we’re eating or stress in our lifestyle, and you create oxidation, it’s almost like rust on a car, that’s what oxidizes iron. And you basically create rust on your lipoproteins. That’s the damaging kind of problem. It’s not the LDL or the cholesterol itself. So you really want to look at a profile that looks at oxidized LDL or the particle size of the LDL.
(13:13)
And again, this is more than we can get into here, but it’s more important than just pure cholesterol. So don’t ever take your pure cholesterol number for an end all be all, because really is meaningless. It’s good plus bad, which means it’s neutral. So it’s just important to think about that. Inflammatory markers, I’m a big fan of these because these can be predictive as where someone’s headed. Things like CRP, this is just a non-specific inflammatory marker that can indicate a hidden infection like in your jaw, maybe a strep or problem in your throat that you maybe didn’t know about or some infection. And if that’s high, there’s usually a reason, we just have to say, what’s causing it? And it could be anywhere in the body. Homocystine is a great marker of methylation, which is a process that breaks down damaging chemicals. It repairs DNA, and it helps immune system and neurotransmitters like for sleep and mood.
(14:01)
So if you have a high homocystine above about nine, in some cases like with brain issues, we look at below seven. So seven or nine are good numbers to look at. And again, you want it below nine or below seven in some cases. And homocystine tells us, do you have enough methylated B vitamins, methyl B12, methyl folate, B6, and riboflavin? And if you don’t, it’ll start to creep up. I’ve seen people as high as 27 or 30, and we know there’s a massive issue with methylation, which like I said, repairs DNA, prevents cancer, makes neurotransmitters. So super important to have your homocystine below nine.
Betty Rocker (14:37):
I’m just going to interject just for a quick second here to say that these all sound very familiar. I feel like over the last three years you’ve tested all of these things on me. But one of the really interesting layering pieces that you did because of who you are and what you look at is you also compared my results to what my DNA, what my genetic background is, which I think is a really essential piece. If you’re wondering, does someone have the MTHFR gene? Which will allow them to methylate properly, that’s what made me think of that just now. So interesting side note, but also yet another reason why this stuff is so fascinating because we are all so unique and your results might be… You could have the same results as mine, but how we express things and what is going to bother each of us, or make each of us thrive could be different because of our genetics.
Dr. Jill Carnahan (15:37):
Yes. This is so true and so important because again, when there’s a homocystine issue, I’m like, “Okay, what caused that?” And if someone… You’ve heard of MTHFR, you mentioned that, that’s a common cause of impaired methylation. And so that would be one of the reasons. And if someone has MTHFR, they’re going to require more B vitamins than someone who doesn’t. And I can actually mark progress by how low we get that homocystine. So you can check that in. TMAO, this is the big one in the cardiovascular. If you ever…
Dr. Jill Carnahan (16:00):
TMAO, this is a big one in the cardiovascular. If you’ve ever heard of cardiovascular markers, TMAO is something that your gut metabolizes from choline and carnitine in typically fish or chicken or meats. And it’s kind of, well, it’s not kind of, it is a risk factor for heart disease. However, it’s the gut microbiome that produces it. So say you have a high TMAO and your doctor checked, you’re like, “Oh no, I need to cut out fish and chicken and all these wonderful proteins that are clean.” The truth might be maybe temporarily, but the real root there is microbiome. So you can go back to the microbiome, fix the microbiome, change the microbiome. And sometimes it’s not the carnitine, which is a great nutrient, choline, which is a great nutrient or fish, wild salmon for example. But in the conventional world, we say those things will increase TMAO so you need to avoid them all. And the truth is you fix the microbiome. That’s a big one.
Betty Rocker (16:53):
And we just got to talk to Dr. Pedre recently all about gut health, which was so helpful. And it’s really intriguing and important for us to learn as much as we can about how our bodies work and how to take care of them through just our day-to-day life practices. I have not yet met one doctor who I’ve interviewed or talked to or worked with who didn’t tell me how important it was to pay attention to my own practices in my own day-to-day life. That whatever treatment protocol they had me on, I was also going to need to pay attention to my sleep, pay attention to my stress levels. What was I eating? Was I paying attention to my gut health? Was I exercising? Those pieces are the responsibility of each patient to the best of their ability. All or something guys, not all or nothing.
Dr. Jill Carnahan (17:38):
Right.
Betty Rocker (17:38):
But it’s like all of these tests are so great, but then what are we doing ourselves on the other side of that? Like you mentioned the gut microbiome, which it’s just a favorite topic around here because it’s such an important part of the other side of we eat something and how does that influence our gut? And then how does the gut talk to the brain and the hormones and then what shows up on a blood test. You’re talking about this TMAO, how interesting that connection is. It’s all so interconnected.
Dr. Jill Carnahan (18:09):
Because we never used to think, like the gut microbiome kind of back burner, it’s important. But now we realize so many of the drugs we use, so many of the chemicals we get exposed to, they don’t necessarily affect our cells, but they affect our gut, which then affects our body. So it’s very relevant. Those are just some of the inflammatory markers. There’s even more, but those are the big ones. Having metals are a big deal because we’re all getting more and more exposure.
Betty Rocker (18:30):
I’m glad you brought that up.
Dr. Jill Carnahan (18:32):
Especially out here with wildfires, we know that there’s chemicals in the building materials that are being burnt. And California, Colorado have been particularly affected last year and the last several years by wildfires. And wildfires we saw, you’ll be surprised but maybe not surprised, but after the wildfires, we saw these kinds of inflammatory markers in people’s blood in my community where there was lots of houses that were burned that looked like someone who had massive mold exposure because the same kind of inflammation. So heavy metals are a big deal, and there’s several ways, I’ll try to be real simple with this. You can test these in the blood. They’re going to be recent exposure. They’re not going to be body burdened. So it’s very easy to get a heavy metal test in your blood and it might show if you had shark and swordfish and some hot tuna and eating some high mercury fish. You might see mercury from recent exposure, but it won’t really test your body burden. To get the body burden, you’re going to want to do urinary excretion, and you’re probably going to want to do that with a challenge with your doctor’s prescription for DMSA. That’s a little more complicated, but at the very basic, you can get blood tests through any regular lab of heavy metals. And that’s important.
Betty Rocker (19:40):
That’s so important. I remember back when I first got my sauna, my infrared sauna, I had really high levels of different metals. And after I got tested again a year later and they had gone down so much, it was amazing. When I actually focused on, it was a big deal. So that’s an important test because-
Dr. Jill Carnahan (20:00):
And I love that you-
Betty Rocker (20:01):
Consequences when you have high levels of metals in your system.
Dr. Jill Carnahan (20:05):
Yeah, these really affect the kidneys and function of brain that can deposit aluminum that’s been shown to be associated with Alzheimer’s. So kind of some really nasty things. And I love what you said too, because what happens when we start to detox, often mold will trash our detox system. And in the moment if we’ve had a mold exposure, some really toxic exposure, we’ll look really toxic with metals. But as we sauna and detox and get this out, the metals will come out. But it actually, because our detox system’s working, it’s not as big a deal as it was when we were really toxic with mold or other things like that.
Betty Rocker (20:36):
Yeah. Side note for those of you who are really curious about the mold conversation on Dr. Jill and I had that last season. You should listen to both of our episodes together, but that was a deep conversation that we had about my current treatment plan at the time and all the protocols. So if that’s a topic of interest, go listen to that episode because it’s a great one and thanks for that.
Dr. Jill Carnahan (20:58):
Yeah, we went deep didn’t we? [inaudible 00:21:01], of course you’ve heard about. This is probably more talked about than anything else, but let me just be real brief and quick. TSH alone will not do it. It will not tell you the full picture. You need to look at T3, 3T3, T4, 3T4, and then all your thyroid antibodies and that way you get a big picture of what’s in the blood, what’s active in your thyroid. Do you have enough both T3, T4, are you converting? And do you have the brake pedal on that, which is reverse T3? And by looking at that with a doc who knows what they’re doing, you can kind of see, you might feel like your hypothyroid, but your TSH is normal. But then you have very low T4 or T3 and you really are functionally hypothyroid. But you won’t catch that unless you do that full panel with the thyroid.
Betty Rocker (21:43):
That’s a big one I think a lot of people struggle with because they’ll come to me and they’ll say, “But I went and got my thyroid tested and Doc says my thyroid’s normal.” And we know that maybe they haven’t looked at everything that you just went over or there’s just not as much depth in the looking. So that’s an important topic.
Dr. Jill Carnahan (22:05):
It is. Years ago after I had Celiac and Crohn’s and all these things, I was measuring normal TSH and I had so low of T4 that finally went into [inaudible 00:22:14], “Jill, you are severely hypothyroid. You don’t have any T4.” And even at that time I was just getting into functional medicine and I sort of realized, oh, some people can have this. It’s basically dysfunction between the talking of the hypothalamic pituitary and your actual thyroid gland and mine wasn’t communicating. So I actually had a significant hypothyroid and it wasn’t measurable on TSH.
Betty Rocker (22:35):
Interesting. Right. And you’re mentioning that transition that you made from being a conventional medical doctor to becoming a functional medicine doctor. There’s a lot of additional training. There’s a lot of additional school and reading and research and all this certifications and stuff you have to go through. And you’re so helpful because you’re like, “Hey, I went from this where we didn’t know what the issue was to this deeper level of research and that’s when we were able to uncover it.” And I think this is why I really enjoy talking to functional medicine doctors so much because there is such a depth that you bring to the practice of healing people. It’s a real art and science kind of combined I think.
Dr. Jill Carnahan (23:18):
Thank you. Yeah, it does. It’s a lot deeper. And the funny thing is most of your docs who are trained in medical school learn the biochemistry at some point, but then they kind of went to more prescription, and again, nothing wrong with that. Drugs are appropriate, but there’s way more. So if you’re not getting more answered-
Betty Rocker (23:31):
There’s more.
Dr. Jill Carnahan (23:32):
Yeah, keep asking questions. Don’t be afraid of that. Hormones. Oh, we could do a whole episode on hormones, but we’ll talk real briefly. So you can do blood work hormones and they’re decently good and they’re actually a great way to get covered by insurance where you really look at levels. Typically I’ll recommend free and total testosterone. Estradiol, may be also estrone, which is E1 and Estriol, which is E3. And estradiol is E2. So those would be all the estrogens that are the main ones we use. And then DHEAS, which is the type of DHEA you measure in the blood. Cortisol is really important. And usually we do morning cortisol before 9:00 AM because there’s kind of a standard. And you can do pregnenolone, so you can go a little deeper. Those things are easily available.
(24:13)
But if you happen to be transdermally applying hormones, you’re not going to see that show up in the blood as much cause it goes into the tissues. So if you’re measuring how you’re responding to a hormone that you’re putting on your skin, the blood is probably not going to show you what you want to see. And in that case, then you go to something like, Dutch Hormones is my favorite company. I have no association with them, but we’ve done that before. They look at all the different metabolites. It’s like a map. You’re looking at this map of all the hormones. And I can tell as a doctor what they’re doing with the hormones I’m giving them. And because it’s measured in the urine, it’s more accurate for tissue levels. So if you are applying hormones to your skin, you’re going to want to do this kind of test. Now this is typically outside of insurance, but it’s a few hundred dollars. It’s not crazy expensive. And there’s multiple different companies. I just mentioned one that we use frequently.
Betty Rocker (25:00):
That’s one that you and I have used frequently. And the Dutch might be something like, first we’re talking about blood panels that you may want to establish a baseline with.
Dr. Jill Carnahan (25:09):
Yes, yes.
Betty Rocker (25:09):
Jill’s giving you a bonus one. And this might be something for follow up or if you notice that something might be off in what you’re looking at in your blood work, then maybe it’s time to talk to your doctor about going deeper and doing the Dutch test, which is exactly why we used it for myself when we were trying to balance my hormones. So that’s super helpful. And we are going to talk more about some specific things about hormones coming up here in a few minutes. But I want to let you get through the rest of whatever else you would tell us to test because this is incredibly valuable.
Dr. Jill Carnahan (25:42):
Yeah, so hang with me. These are all super important and the last few will go a little quicker. So autoimmunity, there’s ways to screen, so we call it predictive autoimmune. And there’s one that was real common your doctors probably tried, if you’ve ever asked for autoimmune, it’s called ANA, antinuclear antibody. We think of this as kind of the doorway into autoimmune disease. And you might have a positive ANA, but really feel okay or not be testing for rheumatoid arthritis or anything like that. But if you have that positive an ANA, that means your body’s already developing antibodies to your own mitochondria, your tissues. It’s actually two part of the DNA of the cells. So that’s telling us there’s something brewing even if you don’t have a full autoimmune disease. So as we talk about trajectory and where you’re walking on that trajectory, this would be a sign if your ANA is positive that you need to look deeper maybe at the gut, maybe at the immune system. And there’s ways to do that to say what’s triggering my immune system to start to attack myself. And so that just tells you, do I have a proneness to develop autoimmunity? And if you do, you better start looking at things that are triggers so that you don’t have to go into full-blown autoimmune disease.
Betty Rocker (26:46):
I can already feel like the sort of anxiety that some of my listeners may have in listening to you go over all this because they feel, “Oh no, what if I have to read these results myself?” I just wanted to share a personal share about my own results. Because when I’ve gotten them back, I usually get them back before Dr. Jill does or around the same time that she’s going to get them. And we may not have a check-in visit for a couple of weeks. But what I’ve found is that these results are quite clear. They’re usually showing you a range of what’s normal on the chart, but then all it’s taken me is a brief Google search to find out a lot more about what that specific marker is testing, about what positive and negative and the spectrum of that is. So I feel like I’ve been really proactive in being a patient.
(27:36)
And even if I wasn’t working with you, I would know a lot just from looking at my own labs. And even if I had maybe a different type of doctor who wasn’t a functional medicine doctor, I would still be a lot more educated and a lot more able to converse about these results. Because these labs, when you get them back, you can see. They give you quite a lot of information about everything and then you can just go look up yourself. I mean, you do these days really have to take your health into your own hands. Even Dr. Jill working with me, she doesn’t have every answer I ever need. A lot of it comes from us working together and dialoguing and figuring it out and looking at data. But that’s something you can do too. You can take your health into your own hands. I hope you get to work with a wonderful doctor like Dr. Jill. But if you don’t have someone, this is still accessible. I guess I just want to make that clear.
Dr. Jill Carnahan (28:32):
I love that because you’re right. And nowadays, and a couple years ago there was new law. So before the doctors would keep the labs and the patient didn’t have access, which I think was terrible. I think this is the best thing that ever happened. Now it’s actually a law that you as a patient, whether or not you see physician for follow up or no matter when is your follow-up, you get access to the labs you. That’s your right. So don’t be afraid to ask. If the lab doesn’t release them to you, which they should, don’t be afraid to ask your doctor before the visit or if you don’t end up doing a follow- up, whatever it is, you have the right to this data. It’s yours. So, really important.
Betty Rocker (29:04):
Thank you. Okay, please continue.
Dr. Jill Carnahan (29:07):
Okay. Yeah. So immunoglobulin levels, this is something that’s not common and I find to be absolutely essentials. This is our antibodies, our B cells make antibodies, IgG, IgM, IgA, IgE. And they all do different things and your doc’s going to know what they do. But just knowing that you have normal levels of all of these is really important because if you don’t, that’s a sign of an immune deficiency. Like especially a low IgG level, that’s your total antibodies. And I always check this because a lot of people who are suffering from chronic infections or not feeling well, no docs ever checked this. And I have discovered dozens and dozens of people with an immune deficiency that no one’s ever diagnosed. And it’s pretty simple and it’s a simple test. It’s not hard to get and it’s affordable.
Betty Rocker (29:51):
That’s very helpful. And I know these are all things I’ve seen on my blood work that you order for me. So it’s just fun to hear you talk through them all and think about how someone would feel if they were hearing this for the first time. Is that the complete panel of stuff that you would order or is there something else?
Dr. Jill Carnahan (30:07):
There’s a couple more.
Betty Rocker (30:08):
Okay.
Dr. Jill Carnahan (30:10):
Yeah, just a two or three more. So metabolically we want to look at, glucose is going to be in your comprehensive metabolic.
Betty Rocker (30:16):
Oh, right.
Dr. Jill Carnahan (30:17):
But I also usually order fasting insulin. That should be less than 5 ideally. And I order A1C, which is an average blood sugar over about three months. That should be less than 5.5. And these are ideals, right? Because you don’t really become diabetic unless they’re a lot higher. And then fasting glucose. So if you look at those three things, your fasting glucose should be below, I like it below 90 and for sure below 100. Your A1C, your average sugar should be below 5.5. And your fasting insulin should be below 5. And if you have those all in order, you’re not walking towards diabetes. And if you don’t have those in order, this is a good sign of maybe why you can’t lose weight or why you’re not feeling well. When you skip a meal, you have a metabolic inflexibility. There’s other things here that can be playing. So that’s just a good check for your metabolic flexibility and if you’re prone to diabetes.
Betty Rocker (31:04):
Thanks for that one.
Dr. Jill Carnahan (31:07):
Yeah, the last, vitamin D, so critical. It is like part of our immune system that’s easy to get. Vitamin D, get that. You should be, I think 50 to 80 is an ideal range. You can tolerate a little higher, so if you’re 90, you just had COVID, you’re fine. Don’t freak out. And below 50, below 40 for sure, there is clear evidence of risk of infection and even death from COVID when it’s below 30. So vitamin D is a huge one. Those are really the basics for serum. I talk about a few other specialty, like micronutrient, celiac testing, fatty acid testing, and a few other things. But the other stuff is usually the specialty labs and some of that other stuff. And if you get all the things that I just talked about, you’re going to have a real good snapshot of where you’re at with health.
Betty Rocker (31:51):
And then as far as following up from that, like say you got that snapshot, you got that nice baseline, and then let’s say we saw some things, we addressed those things, we-
Betty Rocker (32:00):
Say we saw some things, we addressed those things. We’d want to get a follow-up for the specific labs that were abnormal. That would be the standard practice for how we would make sure that the protocol or the treatment that we followed was working for us. And how long, I mean, this is really too general of a question, but is it something that we’d want to test within six months if we followed a treatment? How fast should we expect general treatment protocols to take effect? How soon should we get another test?
Dr. Jill Carnahan (32:29):
Great question. So there’s a few exceptions. Like say there’s a really high CRP. I’m like, oh, something’s going on. Let’s check your dentition, let’s treat with antibiotic if there’s an infection, and then retest in maybe eight weeks. But other than that, what you just said, four to six months is a great standard for retesting. So many people who are pretty normal. A few abnormalities, four to six months is when I would retest.
Betty Rocker (32:51):
And you’d just retest the things that were abnormal, generally speaking, right? And then you might do another full workup maybe every decade, or every five years, or annually? What’s the gold standard for-
Dr. Jill Carnahan (33:03):
I would probably in my patients, because I’m following them, every year. And now maybe not everything, because once I know the pattern… So I’m going to throw out this big net like fishing and say, okay, what are you… So you’re predisposed to metabolic syndrome and inflammation. Well then I’m going to focus on those things, and every year, maybe even every six months, do those. If your thyroid looks great, we might check once a year, but these are still pretty basic. So most of the ones I just described, I will probably do those at least every year for patients.
Betty Rocker (33:31):
That’s helpful. And then let’s shift to my particular audience who’s really interested in their hormone health, and testing their hormone levels, and also treating hormone imbalances that they find. This is the one specific treatment that I’d like to focus on in our conversation, because over the years in working with you, and even other people I’ve worked with, I’ve experienced different types of treatments for when my hormones have been out of balance. For instance, when I was exposed to mold, my hormones really tanked. My testosterone was really low, my estradiol was, specifically of the three different estrogens in your body, that one was super low. And that’s the one that helps us make muscle and have drive. And that’s the one you don’t want to be low. So we treated me in a variety of different ways.
(34:17)
We used creams for the most part, since I tended to want those, and responded well to them. And then I slowly transitioned off of all of those supplements, and got onto I’m calling them supplements, but they are supplemental. They’re more prescriptions. I transitioned into using adaptogenic herbs and supplements, and I was at a great place with all of those until I got COVID. And then I tanked again, because as you’ve educated me, COVID is one of those things that really attacks our hormone levels, especially after women my age, in my mid 40s, have had COVID. So I’m just, the floor is yours. Talk to us about the different treatment options available for us as women who need hormone therapy support, why you recommend different things over others. And then we should also talk about how COVID attacks us.
Dr. Jill Carnahan (35:07):
And I’m going to weave that in the beginning because I think many listeners, you’re going to… It’s so relevant. Many of you are like, what just happened after COVID? I recovered, it wasn’t a severe illness, but COVID has this really significant impact on our immune systems, and particularly our adrenals. And if you’re in your 40s or 50s, what’s happening is you’re maybe in perimenopause, or you’re maybe kind of hanging in there with normal cycles. And I’ve seen over and over again, if someone’s on that borderline post-COVID they dump into menopause. They tip over that cliff. And the reason for that is COVID has a particularly strong effect on the adrenals. And when we are going towards menopause, our adrenal glands actually pick up the slack. So when our ovaries stop producing that amount of estrogen and progesterone that we need for our cyclical cycles from 30s and 40s, early 40s, our adrenals will start to kick in.
(35:56)
And we can actually go through perimenopause for years, for three, four, five years, if our adrenals are really strong. And those with strongest adrenals are going to be the ones that, “Oh, I don’t really notice menopause symptoms, I feel fine.” Because their adrenals just, it’s just very gentle from the ovaries to the adrenals, and they pick it up and take the ball. It’s like passing the ball, right? And so post-menopausal, our adrenals carry the load of producing hormones for us, and we definitely go down. But what we’ve seen, the reason any virus, even like Epstein-Barr or CMV could also do this, but because so many people have been affected by COVID, we’re seeing a large amount of women in their 40s and 50s that after COVID, they go right into menopause, because their adrenals are in a weakened state. So that’s the framework of this, and why people are seeing more issues after. And then what to do about it?
(36:41)
Well, like I said, you can have your blood work tested by your doctor, and usually it’s covered. You can go deeper with the Dutch, or any urine or saliva tests that will actually look at deeper levels, and you want to see what’s happening. And then you can get a plan together to replace that. One of the things I was so proud of you doing is you did an amazing job with adaptogenic herbs to really support. And I think a lot of women, if they’re teetering and they’re not fully blown, I prefer to do herbs because herbs are this warm blanket for our body and hormones, and they’re very gentle. They work. If you’re high cortisol, they might lower it. If you have low cortisol, they might raise it, but they work synergistically with your own body very gently. But then sometimes we fall off the cliff, I do that too, and we need a stronger support.
Betty Rocker (37:28):
Yes. Yeah, no, and I’m glad you’re sharing, because I’ve really wanted to talk about my own experience because I feel like it mirrored so many people. And maybe if it wasn’t the same as someone else, there’s something relative about it. And I loved the adaptogens, because it wasn’t… I feel like you take a pill or you take a cream, and you get a faster response. I feel like the creams actually you can… They’re gentle too. I guess I’m thinking about, you’ve got suppositories, you’ve got things you insert under the skin. You’ve got a pill you can take, you’ve got a cream you can apply. There’s all these different applications for helping us shift our hormones in the direction we want. But then the adaptogens really felt like they were slower. They worked slower. I had to be patient. And that’s why I was glad I used them towards the tail end of my cream treatment that I was on. But anyway, thanks for that.
Dr. Jill Carnahan (38:21):
Well, that’s why I’m so proud of you, because I thought that’s such, that’s actually a way better synergistically, harmonious way with our own bodies to nurture us. Because I always say hormones are sledgehammers. There’s nothing gentle about them. And they’re appropriate for if you’re menopausal and you need support, it protects the brain, it protects the heart. There’s so many good things about them. They’re very appropriate, but they are big guns. So I always prefer the gentler things. Let’s talk a little bit about applications because it does matter. Oral is my least preferred for testosterone, for estrogen, not for progesterone. Progesterone orally is very effective, and will convert to GABA. So if you have sleep issues, which is really common perimenopausally, oral progesterone is safe and effective, and I don’t worry about it, but estrogen and testosterone have to go through the phase two of the liver and they get metabolized.
(39:10)
And you actually have to give higher doses orally to get through that liver first pass, and then what’s in your tissues and what’s used. And there’s a little bit more risk of bad effects like clotting for estrogens, or even issues with breast or breast cancer, things like that, when you take them orally. So some people need that, but it’s my least favorite way. Transdermally is the most natural. And you can do this in creams. There’s commercially available patches, and those things go right into your tissues and they act most closely like our ovaries do, just releasing them into your tissues. So that’s a very safe way. It bypasses the liver so you don’t have that liver risk of stressing your liver, or even toxicity, or breast issues as much. And you can do testosterone, estradiol, or bias any sort of estriol… sorry, estradiol-estriol combo, or progesterone transdermally on the skin.
(40:01)
You mentioned pellets. Pellets are very convenient. People love them most commonly as testosterone pellets. But you can get other hormones like progestins, or progesterones, or estrogen. The number one question you want to ask your doctor is, “Are they bioidentical?” Because you want the same thing your body produces, even if it’s in a patch. You can get bioidentical estradiol, even though it’s a patch that looks like a prescription, but you don’t want progestin, which is synthetic progesterone. It’s not the same. So you want to make sure whatever you’re using, patches, or creams, or oral, it’s bioidentical. And then those pellets, those usually last about three months. And the pros and cons are you get it once, and then boom, you’re good to go. But what I see on that is it’s a spike of a curve, like say [inaudible 00:40:47], and you go way too high beginning, and then by the last two or three months, you’re tapering off to too low. And if it doesn’t work, like say all of a sudden you grow a beard or you’re losing you’re-
Betty Rocker (40:57):
You can’t take it out. You can’t stop.
Dr. Jill Carnahan (40:59):
Right, right, right. So I am not a fan of pellets, even though people love them, and I have practitioner friends that do a great job. It’s not a wrong thing to do, but you have to be aware it’s in your system for three months. And if you go wrong and you get too much or too little, you can’t really change it.
Betty Rocker (41:14):
Yeah, I’ve been really, I’ve had a lot of success using the creams. Just one of the things I liked so much about the creams personally was how we were able to adjust the doses so quickly with a cream. You can use more, you can use less depending on the response that you’re having. And that felt really supportive to me, and why we saw such a good response. I also really liked the new, since I had mentioned previously, I had COVID, and my estrogen levels had tanked along with my testosterone, and symptoms I was experiencing were afternoon fatigue, and I started to just put on body fat more easily again, which was surprising, because I had really gotten to a place where I was just in a maintenance mode again with my training, and my nutrition, and all of those practices. So I noticed when I was starting to easily put on a little extra body fat. So those were just some simple signs for me that… And then I was starting to have hot flashes, and-
Dr. Jill Carnahan (42:17):
Yes.
Betty Rocker (42:18):
I was like, oh my gosh, I thought I got rid of these when we fixed my hormones last time. And that was my sign. I was like, “Dr. Jill, what do we do?” And I was going to say, I really liked this new estrogen drops. They’re also a transdermal that you had recommended to me. I had never heard of them before. Basically, there were a lot of different options for managing the hormone levels in the body. And this is something that I feel like I want to check in with you about sooner than later.
(42:51)
Because as a patient, I feel like your hormone levels are… It’s a delicate balance. Once you establish a baseline where you notice that they’re abnormal, or something’s gone wrong, I want to be testing again to see, are you having a response? How are you feeling? Let’s look at the blood work again.
Dr. Jill Carnahan (43:25):
So typically six to eight weeks is perfect, four is okay, it’s a little soon, but often you can definitely see changes, and so anywhere between. But I agree, I think it’s so key to follow, because you can say, “This is the standard percentages of hormones that we’re going to use,” but every body is different. And the thing you want to think about, if you have processes with cytochrome issues, which again, this goes to genetics. So I can look at someone’s genes and see a C1B, which is related to hormone metabolism, and I know, “Oh, they’re going to not break down that estrogen as quickly as someone else. And because of that, I need to maybe give them a lower dose, or we could become…” Because too much estrogen is a risk of endocrine related cancers like endometrial breast.
(44:06)
The one thing is the Women’s Health Initiative, which came out 20 years ago, initially started to look at safety and they said there was all this risk. But the final say on that data is actually that hormones are quite safe, especially if you start them right around the time of perimenopause, even with breast cancer. So I feel like I want to always empower women to feel not scared. I am a breast cancer survivor, so I speak from a very important place, knowing I had breast cancer aggressively at 25, and I replaced my hormones in an appropriate way. And I feel that safe to do it on my own body. And so I want to encourage patients that as long as you’re watching it, working with a doctor who knows what they’re doing, many cases are safe. And again, it depends on estrogen receptors. I don’t want to go into all that. So if you’ve had breast cancer, absolutely check with your doctor before starting hormones. But there is ways to safely help your symptoms, even if you’ve had breast cancer, and especially if you’re ways out, to five or 10 years out.
Betty Rocker (45:03):
That’s a great framework and really valuable information, both how we’re testing our hormones, how frequently we’re testing. That’s really helpful advice. And for all of that great information about the different types of treatments available for women. You can read this article where I researched on my blog, there’s an article about the adaptogens that I was particularly interested in researching at the time, and there’s a lot of information about how they all interact with your body. So that’s a great resource if you’re wanting to dabble in that. But I guess another thing I really love about the practice of functional medicine is that you’re not limited by just the drug.
(45:56)
You really have this broad palette that you draw from that takes into account a lot of different things that could be beneficial for someone’s body. So I love that that’s the focus, that there is such a broad focus. What can help this individual person? And we’re looking at the root of what’s potentially creating this abnormality in their system. We’re looking at the framework of their genetic background in addressing whatever this abnormality is, so that we can really give them a full and comprehensive treatment.
Dr. Jill Carnahan (46:27):
I love that.
Betty Rocker (46:29):
We were talking… Yeah, we were a little bit about COVID. I’m just thinking about the COVID situation, and our immune system tanking. It’s not just our hormones that tank, is it? It’s also our immune system that tanks.
Dr. Jill Carnahan (46:43):
Yeah. So let’s talk about patterns I’m seeing with long COVID. This is actually documented. This is not just Jill’s personal opinion, but we see… But post-COVID in very… In fact, one study recently looked at college kids, which are young and healthy. These are not the people that are dying from COVID, they’re the young ones. They bounce back, they maybe barely know they have it. And they were saying one in five is having some sort of long COVID effect. The patterns I’m seeing are B cells. B cells are cells that create antibodies. So the things that create autoimmunity in someone who’s predisposed, they’re becoming more activated. So there is a risk for many people of developing new onset autoimmunity, or more activation of their autoimmune cells in the long COVID or the post COVID phase.
(47:24)
Number two, T cells. T cells fight cancer. They fight infections, especially viruses. T-cells are being exhausted. I like that term when I’ve heard it in the literature, exhaustion of T-cells. It sounds like the poor things, they’re kind of like, “Oh, this is so hard. We’ve been through this pandemic.” And I just like that. It makes me smile because it kind of is. It’s not like they are gone. It’s not like you don’t have them anymore. They’re just tired. They’re worn out, and they’re not working as well. So we’re seeing a ton of people after COVID develop shingles, or develop reactivation of Epstein-Barr, new onset exhaustion, or fatigue, or other things related to the T-cells not really working. I’ve also sadly seen some people who were fairly controlled with cancer issues…
Dr. Jill Carnahan (48:00):
I’ve also sadly seen some people who were fairly controlled with cancer issues, and their cancer reoccurred, or they had to get more treatment or something. So it affects cancer, it affects viruses, and post-COVID some people are seeing activation there.
(48:13)
The third thing is those adrenal glands we talked about with menopause and perimenopause. Very, very frequently I’m seeing low cortisol, or dysfunction of the adrenals post-COVID as well. And I think when we talk about hormones, that’s one of the reasons why many women are either all of a sudden going into menopause after COVID, or having more issues with hormones.
(48:32)
Because the adrenals, which should pick up the slack, are not working very well. And that might present with feeling overwhelmed, exhausted, more allergies or more reactivity to things. Maybe your gut isn’t as healthy. And people can either gain or lose weight. They can have both extremes. So those are kind of the patterns, the B-cell activation, T-cells exhausted and the cortisol being low. And I see that a lot post-COVID affecting people’s health.
Betty Rocker (48:58):
I was just coaching a woman after one of our training classes in Rock Your Life the other day, that’s the online membership fitness community I have. And she was telling me how after COVID, her allergies had just gone crazy. So that’s just exactly what you’re talking about, and how the body just doesn’t have the same resources available, and it has to rebuild them.
Dr. Jill Carnahan (49:21):
And one thing with that also, that’s absolutely related. And then there’s one more point. It didn’t make mast cells, which are primordial, they kind of protect us from the world. And they’re kind of an early cell, they’re not as well differentiated as the T-cell and the B-cells.
(49:35)
But you’ve probably heard of mast cell activation, I’ve written a ton about it. But the mast cells after COVID absolutely, in some cases, get activated. And that would also explain some of the more allergic congestion, sneezing, even tachycardia or heart palpitations, those can all be related, even leaky gut.
(49:51)
When you produce more histamine from the mast cells, it creates more permeable gut. So it can affect all systems, and that’s common post-COVID as well.
Betty Rocker (50:00):
It’s also common when you’re dealing with mold exposure. I remember you helped to treat me with my masts. I had a whole mast cell response as a result of the mold, and that was one of those things that was really hard to pinpoint. So I’m glad you brought up the mask cell conversation.
(50:14)
So many things out there that can attack our system. And it really brings me back to this baseline of resilience that we all need to build into our body. And we can build resilience in a lot of different ways.
(50:32)
We can build resilience through what I just talked about, our four pillars of health. And the sleep, the stress management, the nutrition, the exercise piece that you guys hear me go on and on about all the time. And that it helps us be a better partner with our practitioner.
(50:45)
But I also think that there’s this side piece, not side piece, there’s a huge piece, our intuition. Our attitude. And this is something you talk about so much. And it’s so refreshing to hear a doctor talk about that aspect of our healing. And I’ve experienced that personally. And working with you, your constant support of me and my intuitive response, and helping me believe in this process.
(51:09)
And I’d just love for you to talk more about that, because I think it’s such an important aspect of healing.
Dr. Jill Carnahan (51:16):
I think many people who go into medicine or go into healing in some profession are actually very intuitive, very creative. This is part of our nature as humans. And I always think of it like right brain, left brain science, faith, masculine, feminine, there’s all these about polarities of life, right?
(51:31)
In medicine, traditionally, it’s actually very, very driven by science and analytical mind, which is beautiful. But we’re taught in medical school to not listen to any of the wisdom of the intuition because that has no validity. And the truth is, they both have validity. And now I feel like this dichotomy is so critical to me helping patients.
(51:50)
Because I know, analytically, how to look at the labs. We just went through that. How to look at the data, the science. I love the science. But this intuitive piece is actually really wise too. And what I’ve learned is over time, if I’m listening and present with a patient and I have this feeling, oh, this feels intuitively like I need to either ask this question, go here or suggest this protocol, and then we always back it up with science.
(52:10)
But we can use that. And then like you said with the patient, I’m asking them, I’m checking in, how does this feel to you? What response did you get with that protocol? What happened with this?
(52:19)
And sometimes they’ll say, yeah, no, doc. I know you said this should work but it didn’t, and I tried this instead. And I just listen to that. Because you know your body as a patient better than any doctor. And I might have the X, Y, Z kind of protocols that work for most people, but if I don’t listen to you, and how your body responded, or how you intuitively feel, I get so much data from that.
(52:40)
And then I can still help guide and say, well, you know what? That makes perfect sense, let’s try this. Or let’s add this, or let’s keep going like you’re going. And I can either validate or say, oh, you know what? I totally get why you did that, but there’s a concern here. Let’s shift and move this way.
(52:53)
But that’s part of the intuition of medicine, and there’s so much power there. Because we can process millions of things of data, whereas our analytical mind can process maybe hundreds or thousands. And you can process so much more on this intuitive level, it’s subconscious. But if you listen to that, there’s, I believe, as much or more healing power and information in the inner bodies.
Betty Rocker (53:19):
And I think earlier I was saying, there’s something that you do where it’s a blending of science and art. There’s an art to the way that you practice medicine. And I feel that that intuitive and peace comes into it. And I started this conversation, this part of our conversation by talking about resilience. And how we build that resilient piece into our bodies, the more we care about how we’re taking care of ourselves. And listening to our own body. And seeking out these answers, and seeking out the care that we’re able to receive.
(53:54)
And also, like you had mentioned earlier, if you don’t like the way that you’re being treated, ask whatever questions you need, but also seek another person if you’re not being treated the way that you want to be treated. I feel like one of the pieces that’s so important in healing, too, is that you feel that the person who’s guiding you, that you trust them.
(54:21)
And how can you trust that person if they don’t trust you with your own body? If they’re constantly making you feel like you don’t know what you’re doing, and that they’re the one with all the power, and they’re the one with all the knowledge and not educating you.
(54:36)
I don’t know. You’ve always guided me to have faith in myself. And that’s a piece that I really appreciate. Is because that self-belief, that faith, that really helps me. I think that’s really helped me in my healing journey. That trust in myself, and that you trust me, and I trust you. And there’s this really important relationship there that I feel like has really accelerated my healing.
(55:01)
Because I believe I’m going to get better. I know it might take a little while. I know that I might have a journey as I go through it and learn things. But I believe that I’m going to get better. And that’s really been helpful.
Dr. Jill Carnahan (55:16):
That is such a core. I love that you’re saying this. Because I feel like in all my journey of cancer, and Crohn’s, and all the stuff I’ve been through and learned through experience, the most powerful lesson is what we’re telling right now.
(55:25)
And what it is is, you have to love yourself. You have to have self-love, and compassion, and take care of yourself and be kind to yourself. But you can’t really love yourself, love your tissues, be grateful for all that your body is taking you through until you trust yourself.
(55:39)
And that self-trust is where I impart that for you, and you impart that to yourself as a patient or a client. Because that trusting your own body has the ability to heal, and that your own body has innate wisdom is so important. And you really, really can’t love yourself until you trust yourself. So it’s core.
Betty Rocker (55:58):
Yeah. It’s core and you need, but I think you also … That’s what I love about you, is that you blend the science with this. Because the landscape of understanding of what’s going on in my body below the surface, the greater my capacity to love that process and to understand that process, which creates all this space for me to trust the process.
(56:18)
So I think it’s important, how you’re holding the space for this conversation that doesn’t have to be one or the other. That it can be both. And because women are so empathetic, and intuitive. And these are gifts and strengths that we have. And I think when we blend them with the scientific aspect of things, we know science is always evolving.
Dr. Jill Carnahan (56:41):
Exactly.
Betty Rocker (56:41):
Look how much research wasn’t done on women in the past. Look how much more we’re learning these days about what’s the right way to treat people. I mean, it’s amazing.
(56:48)
So anyway, I wanted to touch on that because of how much your new book, Unexpected, has such a big, it carries many of these themes through and really draws from your experience of, what is it? 20 years of practicing?
Dr. Jill Carnahan (57:02):
Yes.
Betty Rocker (57:03):
This way. So I just really appreciate all these aspects of medicine. And I appreciate how healthy I am, and thank you for all of your wonderful care of me and all of the other patients who you serve. And all the free information that you share on your blog, here in your new wonderful book, which we will link to and the show notes as well.
(57:24)
And you can look it up on, I’m sure you can find it on Amazon, just look for Unexpected and Dr. Jill Carnahan. And you can read more about Dr. Jill’s personal story as well, like I was saying at the beginning. It’s really, I really appreciate this conversation so much.
(57:41)
And they can find you on Instagram at Dr Jill Carnahan, right?
Dr. Jill Carnahan (57:47):
Carnahan, yep. Jill Carnahan exactly, thank you.
Betty Rocker (57:48):
And you’re on Facebook, and you even can find her on Facebook. I definitely recommend reading her articles on her website. They’re great material to have at your fingertips. In that, you guys can check out the transcript here on the show notes page for the details of all of the things we just went through with all of those tests. And she’s also got that great blog that you can read as well.
(58:09)
And I really appreciate you framing that for people with the affordability and accessibility of those tests, which we deserve to have access to.
Dr. Jill Carnahan (58:19):
Yes. Amen.
Betty Rocker (58:20):
That’s the thing.
Dr. Jill Carnahan (58:20):
It shouldn’t be just for the, well, this should be something that you can access and get information from your regular doctor, or even yourself, as we said, direct to the lab.
Betty Rocker (58:29):
Yeah. Well, is there anything that we didn’t cover that you would like a last word on?
Dr. Jill Carnahan (58:35):
No. But as we end it there, be kind to yourself is part of that intuition. And I really feel like where our society is going, this is where the healing is going to be.
(58:44)
I mean, all this other stuff is so important. But this next level of trusting and loving yourself, there’s so much power there. So if I just leave you with one thing, start to be kind to yourself. Trust your intuition as far as where it’s guiding you. Find a good doctor to work with. Get the test, and know that you have the power to change this. That you’re not helpless, which sometimes we feel in the midst of these things.
Betty Rocker (59:06):
That is so true. And wise words. And thank you again so much for taking the time to talk to us today. Really appreciate it. And thank you all for listening.
Dr. Jill Carnahan (59:17):
Thank you.
Betty Rocker:
I just wanted to mention real quick that one of the most common mistakes I see women making when it comes to their health and fitness goals is putting too much emphasis on their workouts and not prioritizing nutrition or sleep or stress management.
Because one workout makes us feel good, a lot of us think more workouts will make us feel better and give us more results. So we get into this no days off mentality, sometimes going for two workouts a day, and endlessly pouring our valuable energy and time into exercise when that’s actually burning us out and breaking down muscle tissue as the body doesn’t have the building blocks in the form of nutrients or balanced hormones to support all that output.
It’s not really about how much you do, it’s about the way all these important elements, like sleep, nutrition, stress management, and exercise, come together that truly drives your results, supports your body long-term, and as a nice byproduct, produces the results you are looking for physically.
This holistic approach is a long-term sustainable approach that focuses on how you talk to yourself, how you nourish yourself, and how you care for yourself on every level.
And that’s exactly what we focus on in Rock Your Life, my online home workout studio and women’s fitness community. It’s a holistic approach to your health and fitness because you are a whole person.
And in Rock Your Life, you can enjoy the structure of a workout challenge program combined with a balanced guidance around eating healthy, getting good rest, and prioritizing your mental health. I’d love nothing more than to welcome you to our uplifting community.
And to make it easy for you, there’s even a 30-day trial for new members that you can take me up on. No obligation to stay. Just come enjoy the space and see how we can support you in nourishing your mind, loving your body, and rocking your life. Grab the trial at thebettyrocker.com/coaching.


Speaker (59:37):
This podcast is for information purposes only. Statements and views expressed on this podcast are not medical advice. This podcast including Bree Argetsinger, Betty Rocker Inc and the producers disclaim responsibility for any possible adverse effects from the use of information contained here in. Opinions of guests are their own, and this podcast does not endorse or accept responsibility for statements made by guests. This podcast does not make any representations or warranties about guest qualifications or credibility. Individuals on this podcast may have a direct or indirect financial interest in products or services referred to here in. Before starting a new exercise, fitness or health protocol, or if you think you have a medical problem, always consult a licensed physician.
This episode brought to you by Rock Your Life!
Rock Your Life is my online workout studio that you can attend from anywhere you are, and access workout challenge programs, healthy recipes, and get coaching and support in our private women’s fitness community for all 4 Pillars of Health. We provide support and strategies for women in training with their cycle, training in perimenopause and training in menopause.
All of our workouts and training programs include a strong focus on form and alignment to keep you healthy and balanced. You’ll find workout classes to take a la carte of all types, including strength training, HIIT, kickboxing, yoga, barre, mobility and more!
Our workout challenge programs provide a balanced training plan and you can start a challenge anytime within a time frame that works for you! We have challenges in tons of different time ranges, including 15-20, 20-25, 20-30, 30-40, and 45+. We show modifications and welcome all fitness levels!
Join us today and get the support you deserve in an empowering environment!
Thanks for listening! Leave a comment and share your thoughts, and/or leave a podcast review on iTunes!
The post The Lab Tests You Need and Hormone Treatment Options with Dr. Jill Carnahan appeared first on The Betty Rocker.