Fibroids are a common concern. These noncancerous uterine growths can trigger symptoms like heavy bleeding or none at all. Treatment varies, from medications to surgery. Our comprehensive guide clarifies symptoms, risks, and treatments, helping you navigate your options.
Key Takeaways
- Uterine fibroids are noncancerous growths in the uterus that vary in size and type, influenced by factors like hormones, age, race, and lifestyle, requiring tailored treatment options based on individual cases.
- Symptoms of uterine fibroids range from heavy menstrual bleeding, pelvic pain, and urinary issues, with diagnosis potentially made during a routine pelvic exam, but often requiring advanced imaging such as ultrasound or MRI.
- Treatment options include medications, non-surgical procedures like MRI-guided ultrasound, and surgical interventions such as myomectomy or hysterectomy, with specific considerations for preserving fertility in women who wish to conceive.
Exploring Uterine Fibroids
Uterine fibroids develop in the uterus. This fibroid growth is a result of abnormal cell proliferation, inhibited apoptosis, DNA instability, and excessive deposition – factors that can lead to the onset of uterine fibroid symptoms. But what triggers this transformation? Factors such as the following have all been found to influence the growth rate of uterine fibroids and the likelihood of developing them.
- steroid hormones
- high progesterone levels
- genetic mutations
- age
- race
- obesity
- parity
- hypertension
- vitamin D deficiency
- diet
Defining Uterine Fibroids
Scientifically known as leiomyomas, uterine fibroids, also referred to as fibroid tumors, are noncancerous growths composed of smooth muscle cells, fibroblasts, and other materials that can grow in or on the wall of the uterus. Now, these growths aren’t uniform. They can vary in size and structure from woman to woman, and even within the same person.
Given this variety, it becomes imperative to identify the best suited treatment for uterine fibroids in each unique case. Some common treatment options include:
- Medications to help manage symptoms and shrink the fibroids
- Noninvasive procedures such as ultrasound therapy or MRI-guided focused ultrasound surgery
- Minimally invasive procedures like uterine artery embolization or laparoscopic myomectomy
- Surgical removal of the fibroids or the entire uterus (hysterectomy)
It is important to consult with a healthcare professional to determine the most appropriate treatment plan for your specific situation.
Prevalence of Fibroids
Uterine fibroids are far from rare. In fact, about 26 million women between the ages of 15 and 50 in the US are living with these growths. However, the prevalence of uterine fibroids isn’t uniform across all ethnic groups.
For instance, Black women are more likely to develop fibroids compared to their White counterparts, and the process of developing fibroids can vary among individuals.
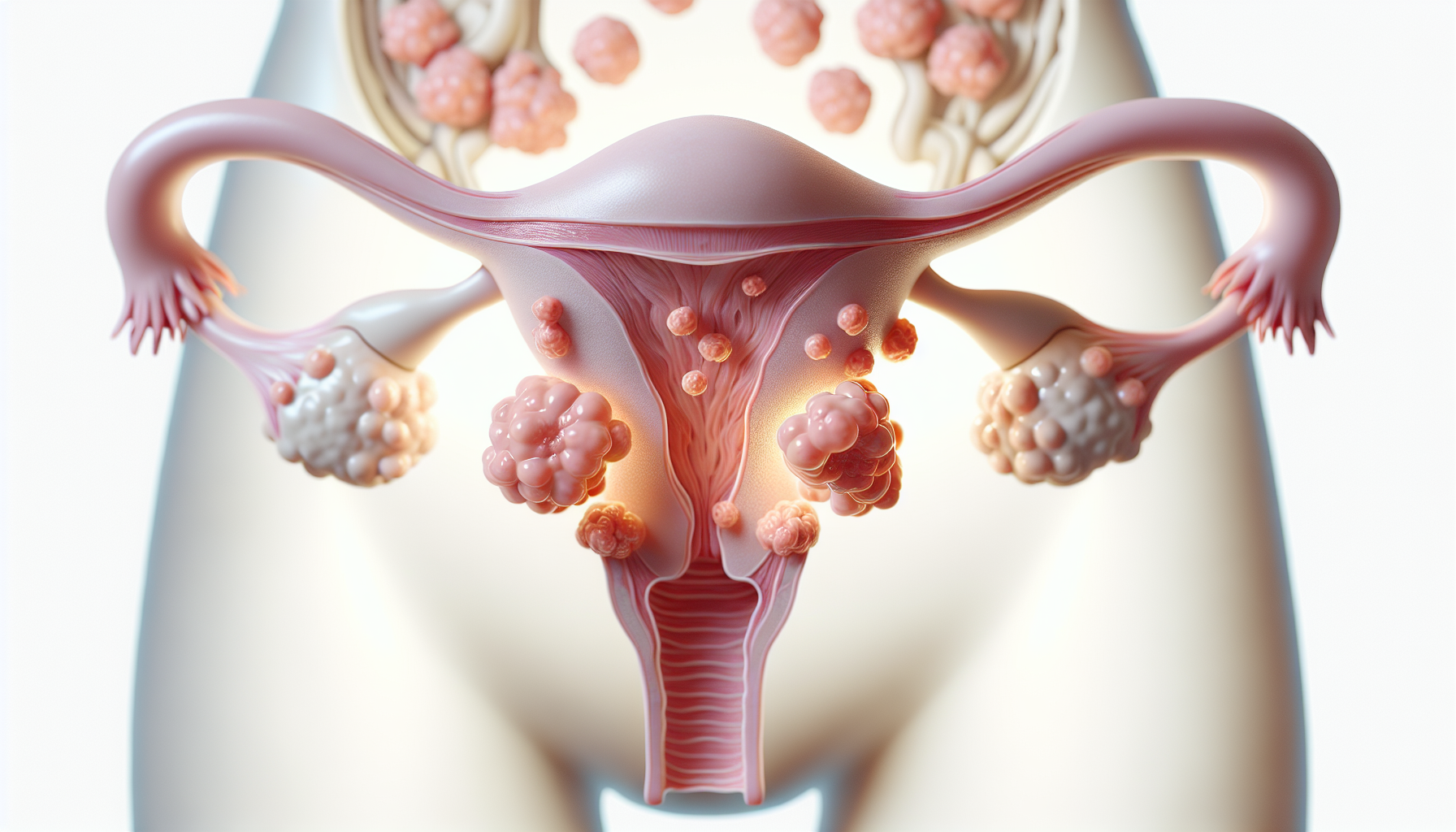
Fibroid Classification
Comprehending the various types of fibroids is key to their effective management. There are four main types of uterine fibroids:
- Subserous fibroids
- Intramural fibroids
- Submucosal fibroids
- Pedunculated fibroids
Each type has its own particular location and characteristics.
Subserous Fibroids
Subserous fibroids are growths that emerge on the outer surface of the uterus, under the serosa. They can cause symptoms like:
- constipation
- lower back pain
- leg pain
- pelvic pain
They can even interfere with the reproductive system by blocking the cervix or fallopian tubes.
Intramural Fibroids
Intramural fibroids:
- Grow within the muscular wall of the uterus
- Can be found on either the front or back wall
- Common form of uterine fibroids
- May affect the overall shape and function of the uterus
Submucosal Fibroids
Submucosal fibroids can cause the following symptoms:
- Heavy flow
- Prolonged periods
- Severe anemia
- Frequent passing of clots
Pedunculated Fibroids
Pedunculated fibroids are growths that develop on a stalk, either inside or outside the uterus. These fibroids can cause severe pain, similar to intense period cramps, and prolonged menstrual bleeding.
Identifying Symptoms
The symptoms of uterine fibroids can vary widely, from heavy menstrual bleeding to bowel and urinary issues. While some women may experience multiple symptoms, others might not display any noticeable signs at all.
Heavy Menstrual Bleeding
Heavy menstrual bleeding is a common symptom of uterine fibroids. This bleeding can lead to anemia, a condition where your body lacks enough red blood cells to carry oxygen to its tissues.
Pelvic Pain and Discomfort
Pelvic pain and discomfort can be a telltale sign of uterine fibroids. Some common symptoms include:
- Lower abdominal pain
- Chronic discomfort in the pelvic area
- A sense of heaviness
- Pressure in the lower abdomen or pelvis
If you are experiencing any of these symptoms, it is important to consult with a healthcare professional for a proper diagnosis and treatment options.
Bowel and Urinary Issues
Fibroids can cause frequent urination, difficulty emptying the bladder, and constipation. This occurs as the fibroids grow and put pressure on the bladder and bowel, leading to these issues.
Diagnosing Uterine Fibroids
Accurate diagnosis of uterine fibroids is a fundamental part of their successful management. While some fibroids can be detected during a routine pelvic exam, others may require more advanced imaging techniques for a clear diagnosis, leading to uterine fibroids diagnosed accurately.
Routine Pelvic Exams
During a routine pelvic exam, doctors may discover abnormalities in the uterine cavity that could indicate the presence of fibroids. However, they usually need to use ultrasound to confirm the diagnosis.
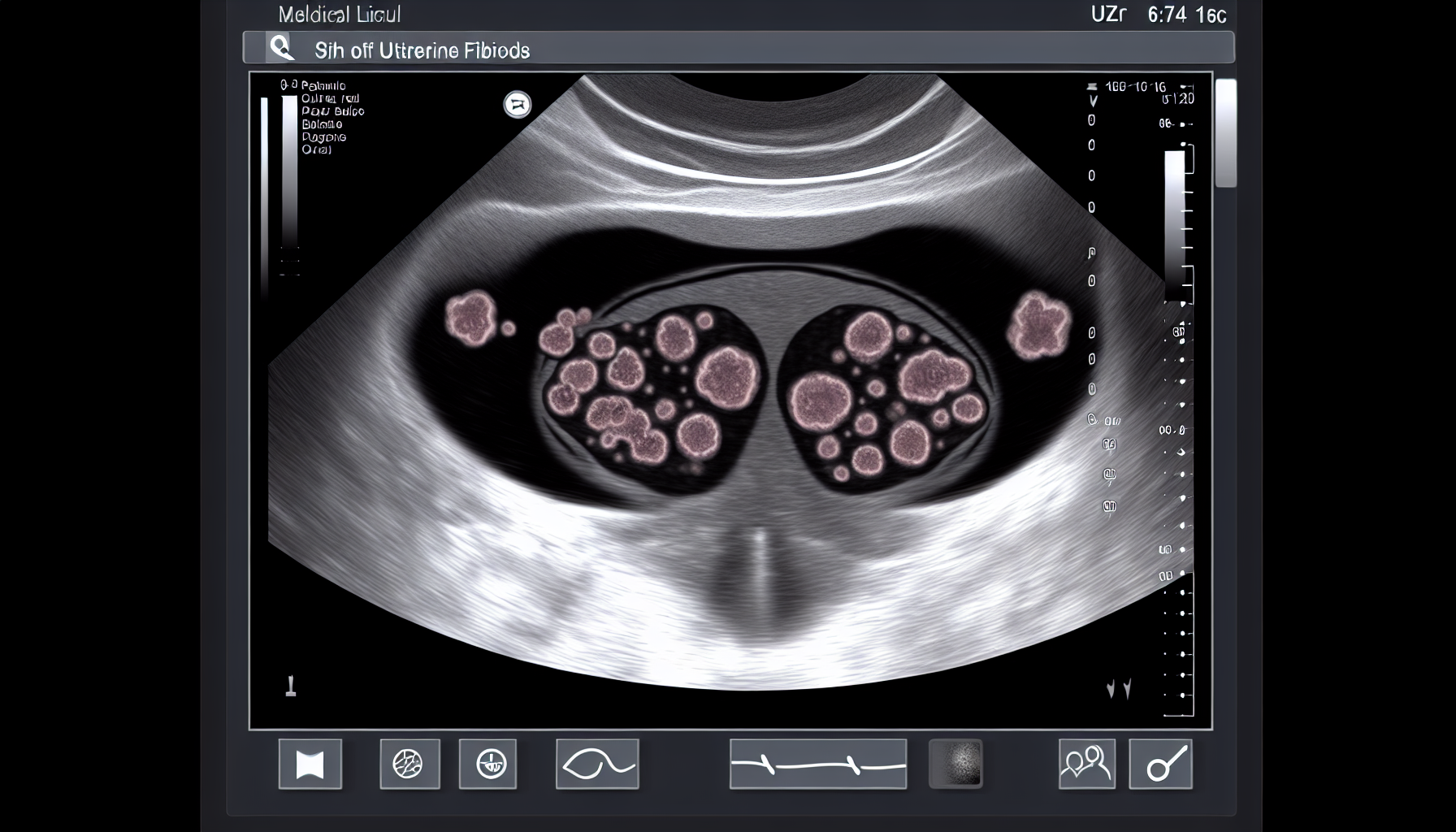
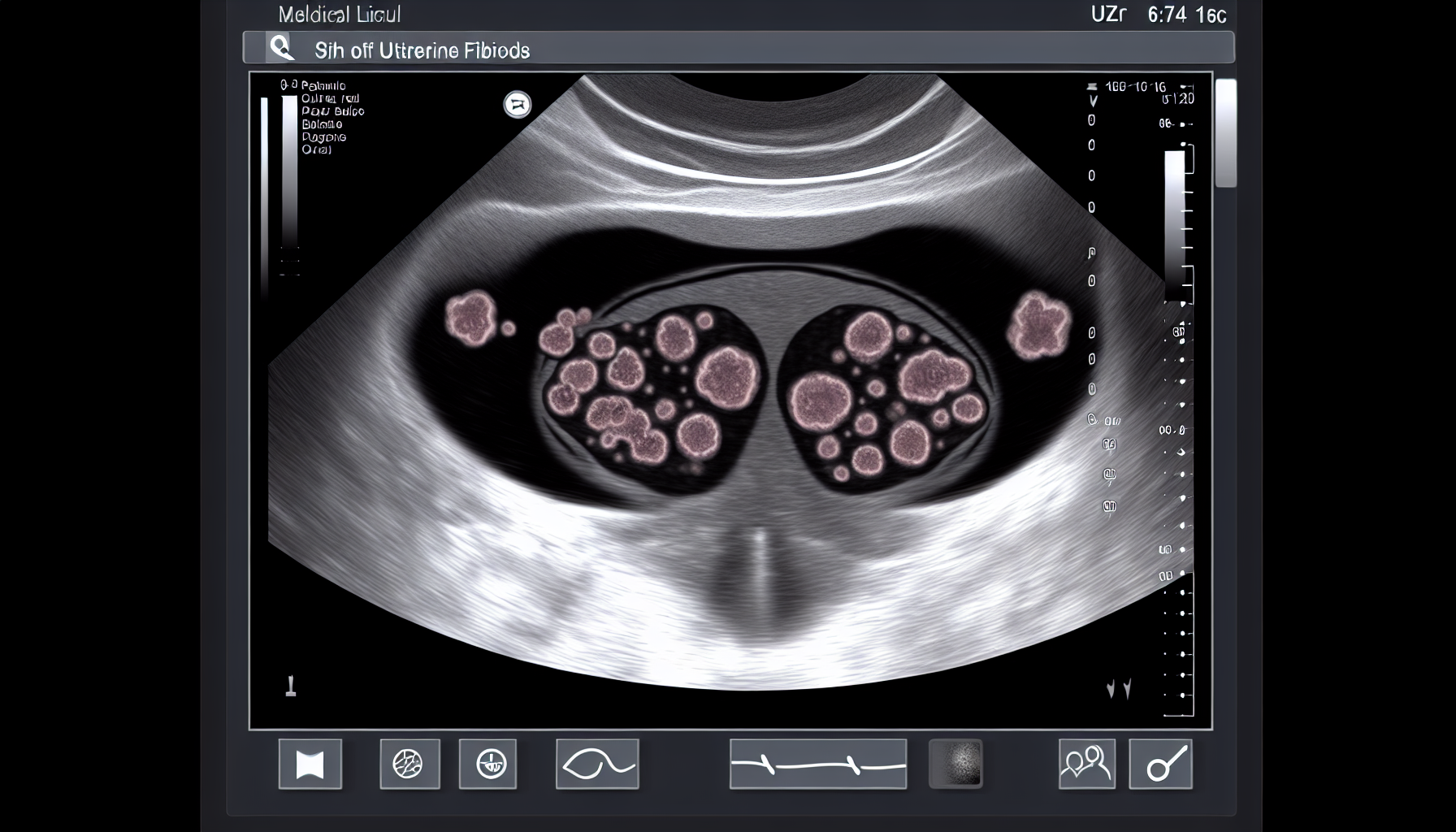
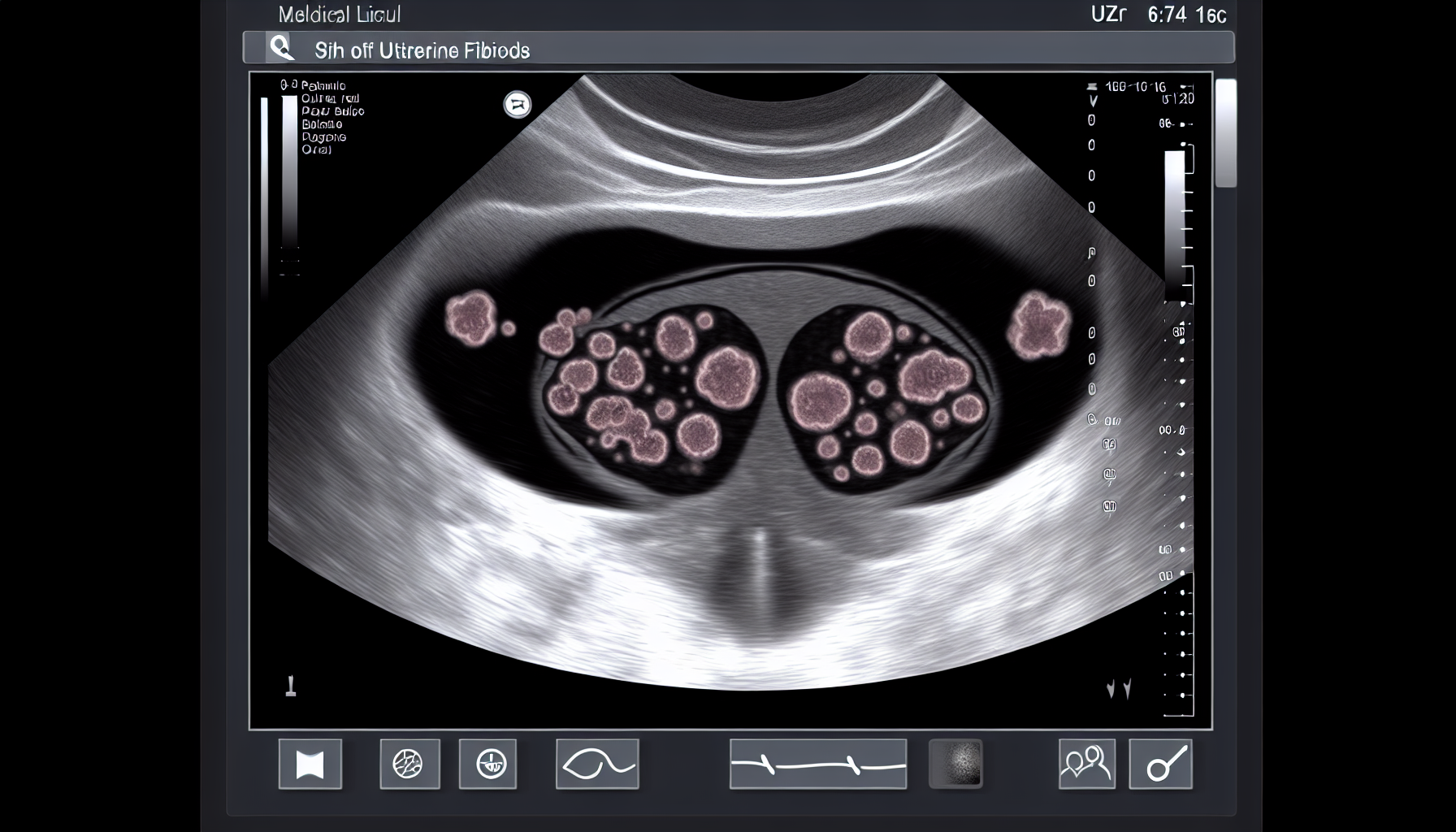
Imaging Techniques
Ultrasound and magnetic resonance imaging (MRI) are the specific imaging techniques used to diagnose uterine fibroids. These imaging techniques enable doctors to view the uterus and its structures clearly, aiding in the accurate identification and diagnosis of fibroids.
Treatment Options
The options to treat uterine fibroids include medications, non-surgical procedures, and surgical interventions, each with its own set of benefits and drawbacks.
Medications
Medications can significantly contribute to managing the symptoms of uterine fibroids. They can help reduce pain and the severity of symptoms, ultimately improving the quality of life for patients.
Non-Surgical Procedures
Non-surgical uterine fibroid treatment options, such as uterine artery embolization, MRI-guided focused ultrasound, and radiofrequency ablation provide less invasive alternatives to treat fibroids. These procedures target and shrink fibroids individually, reducing their size and alleviating symptoms.
Surgical Interventions
Surgical options for fibroids include myomectomy (fibroid removal) and hysterectomy (uterus removal). While these procedures provide a more definitive solution to fibroids, they come with longer recovery periods and potential complications.
Fibroids and Fertility
While most fibroids are harmless to fertility, they can impact fertility and pregnancy in certain cases. Therefore, women planning to conceive should consider treatment options that preserve fertility.
Fibroids and IVF
Fibroids can increase the difficulty of egg retrieval, lower implantation rates, and increase the risk of miscarriage during IVF. Therefore, women with fibroids planning to undergo IVF should consider treatment options that increase the success rate of the procedure.
Treatment Options for Fertility Preservation
Treatment options for women with uterine fibroids who wish to preserve their fertility include:
- Fibroid removal (myomectomy)
- Uterine fibroid embolization (UFE)
- GnRH agonists/antagonists
- A combination of surgical removal, UFE, or medication.
Risk Factors and Prevention
Comprehending the risk factors for uterine fibroids is key to inhibiting their development. This understanding can guide women to make lifestyle changes that can lower their risk.
Known Risk Factors
Factors such as age, weight, and family history have been associated with an increased risk of developing uterine fibroids.
Lifestyle Changes and Prevention
Adopting a healthier lifestyle can play a significant role in preventing the development of uterine fibroids. This includes maintaining a healthy weight, exercising regularly, and following a diet rich in fruits and vegetables.
Summary
Understanding uterine fibroids – their nature, symptoms, risk factors, and treatment options – empowers women to take control of their health. While the journey may be fraught with challenges, armed with knowledge, women can navigate the path to recovery with confidence. Remember, early detection and intervention are paramount, and leading a balanced lifestyle can go a long way in preventing fibroids.
Frequently Asked Questions
What is the main cause of fibroids?
The main cause of fibroids is not known, but studies suggest that genetics and prolonged exposure to estrogen may increase the risk of developing fibroids. So, it’s important to manage estrogen levels for prevention.
What happens if fibroids go untreated?
If left untreated, fibroids can lead to complications like pelvic pain, worsened abnormal bleeding, anemia, and potential infertility in some cases. They may also lead to rare instances of cancer.
How do you fix fibroids?
To fix fibroids, you can consider hormonal therapy like low-dose birth control pills or a hysteroscopy for small fibroids, which is a quick outpatient procedure.
How can I check my fibroids at home?
If you’re experiencing heavy and prolonged menstruation, anemia, pain during intercourse, frequent urination, constipation and/or bloating, or pelvic pain, you may have fibroids and should consult a doctor for further evaluation.
If you need any support or further guidance and would like to speak to someone, drop us a line at info@ivfbabble.com.








