One of the hardest realities to confront on a fertility journey is the possibility of miscarriage. With around 25% of recognized pregnancies ending in loss, miscarriages are much more common than you might think. But why do some people experience recurrent pregnancy loss?
Skip to a section:
- Breaking the Silence
- FAQs About Recurrent Pregnancy Loss
- What is Recurrent Pregnancy Loss (RPL)?
- Diagnosing Recurrent Pregnancy Loss
- Misconceptions About Recurrent Loss
- 7 Possible Causes of Recurrent Miscarriage
- Why We Need to Talk About Loss
- More Resources
CW: This article discusses pregnancy loss in detail
Breaking the Silence
Miscarriage is an incredibly common experience, yet the topic rarely comes up in public discourse. People often feel helpless, ashamed, and broken when their hopes and dreams are dashed by the loss of a pregnancy. It’s difficult to find ways to express the emotions surrounding loss, as it often feels taboo to talk about.
Because it is such an emotional and personal issue, many people choose to keep their feelings to themselves and don’t even share their pain with their closest friends and relatives. While there are starting to be more public conversations around pregnancy loss and there are many great organizations working to reduce the stigma and silence, not knowing what to share (or how to share) prevents many from opening up.
When you suffer through not just one, but two or more losses, confusion, desperation and hopelessness often creep in and cause you to question if your family-building dreams will ever become a reality.
In the interest of increasing visibility and understanding, let’s talk about what we know, what we don’t know, and how fertility treatment and science can provide hope to those struggling with recurrent pregnancy loss.
Note: The terms “miscarriage” and “pregnancy loss” will be used interchangeably in this article.
FAQs About Pregnancy Loss
It is estimated that 1 in 4 recognized pregnancies will end in loss. Because of the silence that surrounds the topic of miscarriage, many people are surprised by how common miscarriages truly are. So why do some pregnancies progress normally and others abruptly end? And why do some people have repeated losses? Let’s answer some of these commonly asked questions.
What is the most common reason for pregnancy loss?
The most common reason for a miscarriage is that the embryo that implanted in the uterus was chromosomally abnormal. In basic terms, a “bad” egg or a “bad” sperm (or both), fertilized to create an embryo that was strong enough to implant in the uterus, but was not viable and did not continue developing into a healthy pregnancy.
These chromosomally unbalanced embryos are referred to as aneuploid. This is an important distinction, because most often the embryo itself arrests its development, rather than being caused by another factor such as the uterine environment. Aneuploid losses are miscarriages that, as doctors, we often explain to patients as your body’s way of taking care of an embryo that was not meant to be.
Note: Aneuploidy is the underlying reason for miscarriages in most cases, and it increases with age.
Hearing that the baby you longed for wasn’t “meant to be” can feel dismissive or painful to hear, but knowing the reason why these little embryos don’t develop into healthy pregnancies can help some grieving patients understand and accept what has happened.
Is miscarriage more common now?
One of the reasons that these losses may seem more frequent is that we are able to detect pregnancies quite early on, particularly when fertility treatment is involved. As pregnancy tests have become more sensitive and other technologies have advanced, recognizing early pregnancies has become more common.
When do most miscarriages occur?
Most miscarriages happen in early pregnancy (the first trimester). This, combined with the fact that tests have become more sensitive, mean that we are not only discovering pregnancies earlier, but that because we are tracking them throughout those early weeks, we now notice more losses as well.
Get the facts from an OB/GYN & fertility doctor:
What is Recurrent Pregnancy Loss (RPL)?
Beyond miscarriages caused by aneuploidy, there are also some patients who have pregnancy losses that are chromosomally normal, termed “euploid.” Some patients have more than their fair share of (euploid) miscarriages.
This condition of repeated miscarriages has a specific clinical term, Recurrent Pregnancy Loss (RPL), and it affects between 1-5% of all women. While aneuploid embryos almost always end up as first trimester losses, they do not count towards the strict diagnosis of RPL as the cause of loss is identifiable.
Recurrent Pregnancy Loss (RPL): The repetitive failure of euploid (chromosomally normal) pregnancy. Two or more failed pregnancies warrants further evaluation, as it exceeds the average pregnancy loss rate.
There are strict inclusion criteria required to receive RPL as a medical diagnosis, and it is important to keep these in mind when speaking with your OB/GYN or fertility specialist. There are many misconceptions among both patients and the medical community about what RPL is and which patients warrant being diagnosed with it.
Let’s examine RPL from an academic, evidence-based perspective and bring clarity to this difficult diagnosis.
Diagnosing Recurrent Pregnancy Loss
Historically, a woman had to experience three first trimester miscarriages to meet the inclusion criteria for a clinical diagnosis of recurrent pregnancy loss. However, research over the last 10 years has extended the diagnosis to those patients experiencing two first trimester miscarriages in a row, in the absence of obvious underlying reasons.
A 2012 clinical guideline from the American Society for Reproductive Medicine (ASRM) states that two non-aneuploid losses are enough to warrant a recurrent pregnancy loss evaluation. While other sources stipulate three losses, two losses is most widely accepted in North America by ASRM and ACOG.
ASRM goes on to define the requirements for RPL in its 2012 Practice Committee Opinion as “Two or more failed pregnancies before 20 weeks gestation. A pregnancy is defined as a clinical pregnancy documented by ultrasonography or histopathologic examination.” Simply put, this does not include any pregnancy that is only recognized by positive blood tests.
Patients may experience grief over any type of pregnancy loss – no matter how far along they are. However, not every miscarriage counts towards the two required for a diagnosis of recurrent pregnancy loss.
Which type of pregnancy loss qualifies?
A biochemical pregnancy (in which the only sign is the pregnancy hormone beta hCG, rises in the bloodstream then drops when the pregnancy fails to progress) can be just as heartbreaking as a loss at 12 weeks or 20 weeks. The same goes for an anembryonic pregnancy, which occurs when there is an empty gestational sac (sometimes called a blighted ovum).
However, the most common type of loss that counts towards the inclusion criteria for RPL is called a missed pregnancy loss. This is a pregnancy where a heartbeat is detected but subsequently ceases to beat. A pregnancy that can be visualized via ultrasound or has tissue associated with it also counts towards the RPL diagnosis. Biochemical and anembryonic pregnancies do not, though they are equally heartbreaking for patients.
Misconceptions About Recurrent Miscarriage
First and foremost, it is important to recognize that we do not find a distinct cause in over 50-60% of patients with recurrent pregnancy loss. While this is very emotionally unsatisfying for both the patient and doctor, there are many misconceptions about what this means that we can now dispel.
Do thrombophilias cause miscarriage?
In the past, the medical community believed that clotting disorders, termed thrombophilias, played a large part in RPL by seeding the micro-vasculature of the placenta with tiny clots. They believed that those clots would then block all the tiny blood vessels and choke off the placenta and pregnancy.
However, research published in well-regarded medical journals (such as ASRM) over the last 5-10 years has concluded that thrombophilias are not related to pregnancy loss. Due to this, they are no longer part of an evidence-based evaluation for RPL.
Randomized prospective studies have shown no difference in miscarriage rates when patients were treated with either aspirin, an injectable blood-thinner, or both. This study and others like it provide evidence-based data that neither blood clotting disorders nor blood-thinners (anti-coagulants) are associated with RPL,
This is difficult for some patients to accept. Being able to point to a specific cause of recurrent loss provides some resolution. Also, blood thinning medications, termed anti-coagulants, can also seem like a straightforward solution to a complex problem. In reality, the only risk these thrombophilias pose is for a woman to have an increased chance of blood clots during pregnancy, not miscarriage.
Do autoimmune disorders cause miscarriage?
We used to believe that autoimmune disorders like Lupus, Rheumatoid arthritis, and Sjogrens disease would activate the body’s immune system to attack a growing pregnancy and its placenta. Published research has ruled out autoimmune disorders as instigators or causes of recurrent pregnancy loss, except in the case of Anti-Phospholipid Syndrome (APS), which we’ll discuss in more depth below.
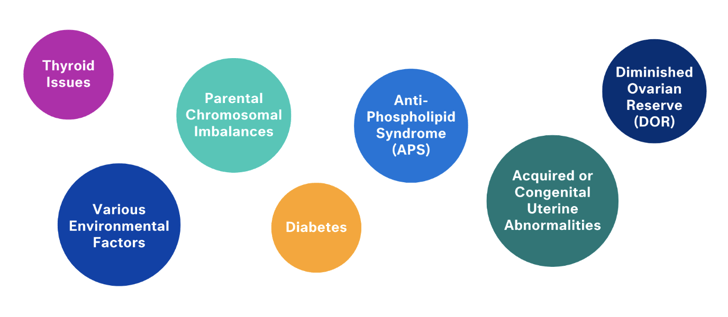
7 Possible Causes of Recurrent Miscarriage
A modern recurrent pregnancy loss evaluation includes six possible causes that need to be looked into. Below, we’ll explore what they are, how they are diagnosed, and what the path forward looks like.
1. Parental Chromosomal Imbalances
Balanced chromosomal translocations in either intended parent account for approximately 1-5% of RPL cases. In these cases, most of the eggs or sperm will be chromosomally unbalanced and lead to repeat pregnancy losses.
Thankfully, in cases of chromosomal translocations, we are now able to test each and every embryo before it is transferred back into the uterus through the use of IVF and a process called preimplantation genetic testing (PGT). This technology is around 98% accurate depending on the particular translocation.
How are they diagnosed? These conditions can be diagnosed through a simple blood test of both intended parents called a Karyotype. Embryos can also be tested using preimplantation genetic testing.
Can PGT decrease miscarriage rates?
2. Acquired or Congenital Uterine Abnormalities
25-35% of all RPL cases can be traced back to an issue with the uterus and endometrial cavity. These include:
Fibroids or Polyps
Fibroids are knots of abnormal muscle that grow in the uterus and can obstruct or compress the womb cavity. Polyps may have this effect as well by interfering with implantation, although this is not as widely accepted in the medical community as it is with fibroids.
How is this diagnosed? Fibroids and polyps can be diagnosed via sonogram with your OB/GYN or fertility specialist. If you have irregular menstrual cycles, pain, or other symptoms, ask your doctor to evaluate you.
Scar Tissue
Whether it’s from a prior surgery, pregnancy loss, infection, or D&C, scar tissue in the endometrial cavity can also interfere with successful implantation and cause other challenges when it comes to conception.
How is this diagnosed? Scar tissue is visible via special ultrasound called a Saline Infusion Sonogram (SIS) and can usually be removed or otherwise corrected with hysteroscopic surgery by a specialized surgeon.
Mullerian (Uterine) Anomalies
Did you know that many women are born with an unusual shape to their uterus? One of the most common (and the one most associated with multiple miscarriages) is a uterine septum, or wall, down the middle of the uterine cavity. This can be corrected by minimally invasive hysteroscopic surgery with a specialist, as described above.
Other Mullerian anomalies include bicornuate, didelphus or unicornuate uterus. These cannot be corrected by surgery and can have varying degrees of negative impact on pregnancy losses. However, they are not mutually exclusive with pregnancy and most people with these conditions go on to be successful in growing their family.
Note: Anatomical issues like these are best treated on an individual basis. Your doctor will help you make a judgment call as to whether surgery is required or helpful to prevent future pregnancy losses.
How are they diagnosed? All Mullerian anomalies are best diagnosed via either a 3D saline sonogram performed by a fertility specialist or an MRI.
3. Diminished Ovarian Reserve (DOR)
Increasing age and DOR are some of the most common underlying causes of recurrent pregnancy loss and the ones I speak about most with patients in the course of routine fertility evaluations and treatments.
Simply put, it means that the reserve strength of the ovaries is diminishing, which leads to decreased oocyte (egg) quantity and quality. DOR leads to fewer eggs “left in the tank,” and also unfortunately means those remaining eggs have a higher chance of being aneuploid (chromosomally unbalanced).
- Patients with DOR will have a harder time getting pregnant and staying pregnant, because of their increased miscarriage risk due to aneuploidy
- A larger percentage of this smaller egg pool will be chromosomally abnormal as you get older
What to do: Ovarian reserve testing is the cornerstone of this diagnosis, so most fertility specialists will order a sonogram of the ovaries and two blood tests (to evaluate your FSH and AMH levels).
Hear one patient’s DOR journey:
4. Diabetes
Uncontrolled diabetes is well known to cause miscarriages, birth defects, and many other pregnancy complications. Diabetes affects the body’s overall functioning (including fertility) and can decrease the chances of a successful, healthy pregnancy.
It’s important to know that pre-diabetes or insulin resistance can cause similar issues as clinically-diagnosed diabetes. Taking action to understand and manage any blood sugar or insulin-related issues early is vital.
What to do: Explore Illume’s Integrated Fertility & Wellness program offerings and reach out for support from our providers so you can optimize your wellbeing and have the healthiest pregnancy possible.
5. Thyroid Issues
Both hyper- and hypo-thyroid conditions are known to be associated with miscarriage and pregnancy complications. A severe untreated thyroid condition can increase the risk of pregnancy loss, impaired fetal brain development, placental abruption and pre-term labor.
- Thyroid Stimulating Hormone (TSH) can be easily checked via bloodwork
- Thyroid imbalances are usually easily treatable and manageable with medication
- As long as your thyroid function is optimized, it should not cause any further issues
What to do: Check with your OB/GYN (or medical endocrinologist if you already know you have a thyroid problem) to get your TSH levels evaluated if you’ve experienced a pregnancy loss in order to get your thyroid under control and help prevent future losses.
6. Environmental Factors
Environmental factors that include smoking, drinking alcohol, recreational drug use, and being extremely over or underweight can all contribute to recurrent pregnancy loss as well. If you are experiencing RPL and using any kind of substances or struggling with weight, consider this a call to action to address these factors.
What are the impacts of smoking?
As you already know, smoking is a big no-no for both fertility and pregnancy. There are conclusive studies that link smoking (even second-hand smoking) to pregnancy loss, as well as lower birth weight and other complications.
Why does being underweight or overweight matter?
Weight extremes (being very over or underweight) are both associated with pregnancy loss, severe pregnancy complications and even stillbirth. It is important to be cared for by a medical team that will treat you holistically to ensure you are metabolically and nutritionally optimized for pregnancy.
What to do: Ask your doctor for support and resources around any of the above environmental factors.
7. Antiphospholipid Syndrome (APS)
We discussed earlier how research has largely disproven autoimmune or blood clotting disorders as a cause of pregnancy loss. However, there is one big exception: Antiphospholipid Syndrome (APS).
This autoimmune condition accounts for up to 15% of miscarriages. Marked by the presence of antibodies in the blood that recognize and attack phospholipid-binding proteins, APS can cause blood clots, pregnancy complications and recurrent pregnancy loss.
While this syndrome does make achieving a healthy pregnancy more difficult, those with APS still have a 70% chance of a successful pregnancy with proper treatment.
How is it diagnosed? APS can be diagnosed via blood clotting tests or antiphospholipid antibody (aPL) tests. If you’ve experienced recurrent losses or blood clots, your doctor may want to evaluate you for APS.
Get support for your journey:
Why We Need to Talk About Loss
While losing a pregnancy is a heartbreakingly common experience, there can be a lot of confusion and misinformation surrounding the topic. Recurrent pregnancy loss carries with it additional levels of frustration, desperation and sadness. This leads those grieving to ask, “Why did this happen, is there something I can do to prevent it, and will it happen again?”
Here’s what to remember:
- Recurrent pregnancy loss is a common (affecting 1-5% of reproductive-aged women) medical condition, and most of the time (50-60%), we do not find a clear cause.
- Outdated beliefs that thrombophillias (blood clotting disorders) and autoimmune disorders cause recurrent pregnancy loss have been proven to be untrue based on current evidence-based research.
- A modern evaluation for recurrent pregnancy loss includes the six factors listed above.
- Up to one in four women who experience pregnancy loss will then go on to have a healthy pregnancy.
- Don’t assume that because you have experienced miscarriage(s), you’ll never be successful.
If you have had more than one loss and can identify any of the factors listed above, then it may be time to look further. Seeking the help of a board-certified reproductive endocrinologist is the best next step to a successful pregnancy.
Even as you navigate the pain of pregnancy loss, I encourage you to try to remain hopeful, because in most cases, achieving a successful pregnancy that ends in a healthy baby is possible.